
Image by IHH Humanitarian Relief Foundation.
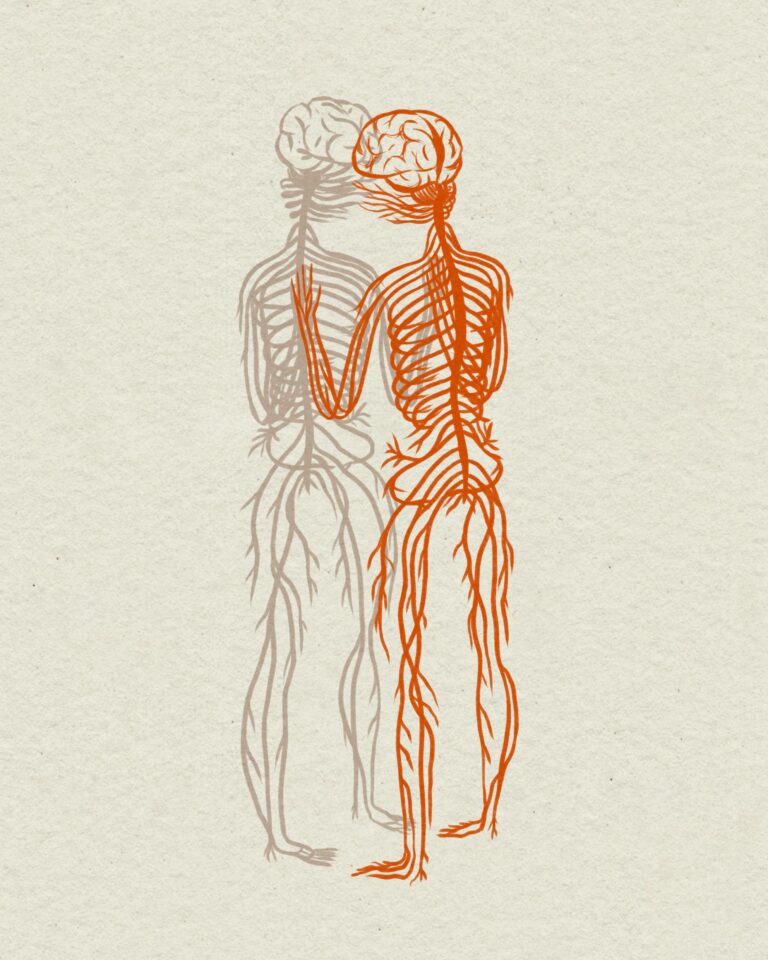
The Culture of Medicine and the Challenges of Compassion
“There is a great compassion deficit in medicine causing suffering to caregivers.”
—Roshi Joan Halifax
For the past 25 years, I have carried with me a vivid memory from my third year of medical school. As I was leaving the emergency room in the early morning hours after one very exhausting night of call, I was thinking of quitting medical school. I was tired of being sleep-deprived, and tired of spending my days and nights immersed in a work culture that I experienced as cold and unfeeling. As I walked through the waiting room toward the exit door, my eyes fell on a woman with a young child on her lap sitting by the door.
Her shabby dress was dirty, her long hair was oily, and her weary eyes looked frightened, intimidated. The child was whimpering, his cheeks were flushed with fever, and I smelled the vomitus on his blanket as I approached.
I knew the ER in that hospital. I knew it was staffed by overworked, cynical residents who were quick to dismiss patients they saw as “dirtballs,” and I immediately felt for her, knowing the kind of treatment she was likely to receive. As my gaze fell on her I remember thinking, with resignation and fatigue, “OK, OK, I will stick this out for you. I am in this for you. You and your child.”
It was not that she was unique. I had seen many patients like her at that hospital, poor and timid women who meekly received whatever was meted out to them, and expressed their gratitude quietly when they were unexpectedly treated with respect and kindness. But this woman appeared at a particularly low moment for me. There she was, beside the exit door, presenting an eloquent symbol of my dilemma: To leave or to stay, to quit or to endure. Her appearance at that moment for some reason drew from me a determination not to quit, and her image came to me from time to time throughout the rest of that tough third year, like an apparition of some spiritual goddess whom I could not let down.

During my admissions interview for medical school in the 1980s, I had drawn blank stares from the interviewers when I spoke with reverence about my desire to be a compassionate healer. My remarks were met by uncomfortable silence. I was naïve about medical culture at the time, and did not anticipate that they would find my idealistic desire to be a healer an embarrassingly puny motivation for a vocation in medicine. They were at least not comfortable talking about it.
Like many medical students who at that time would never have been brave enough to admit it, I entered med school with heart, soul, and mind, a whole self that responded intuitively with awe to the sacred in the wonders of science. Every learning encounter aroused emotions as well as intellect. Throughout much of my medical school training, I felt a powerful force working to alienate me from my heart and soul, from my true and full self, and I struggled the entire time to hold that force at bay.
While I found physiology fascinating, and enjoyed taking histories, doing physical exams, attempting to solve diagnostic mysteries, and planning medical therapies, I also wanted to offer comfort. I needed to connect with my patients. Nowhere in the curriculum was this ever talked about. Despite the fact that we were interacting daily with dying and grieving people, medical school in that era frowned on emotional expression. It ignored the emotional, social, and spiritual needs of the practitioners as well as of the patients.
There was no place for the sensitive self. Sensitivity was actively discouraged. I sat through physiology classes with a professor who drew laughter from the class by describing his sadistic torture of cats. I watched with repulsion the menacing grimace on the face of another basic sciences professor who said to our class, “I will squash you until you are flatter than this coin in my hand.”
The cultural environment was hardly welcoming. Tenderness was scorned.
There was no understanding at my medical school of the arts as having any place in healing. During my internal medicine rotation I remember feeling the urge, when there was a rare quiet moment late at night, to sit at the end of the patient hallway and sing with my guitar. I needed the therapy of music and so did the patients, but music therapy for adult patients was unheard of in that hospital at that time, and I fought the urge, knowing that I would simply be looked upon as crazy.
Looking back now it amazes me that my fellow students and I were not more than a little depressed. One should expect depression from so much repression of one’s whole self, especially coupled with the sleep deprivation that was so much a part of our lives. Were it not for the gentle and insistent prodding of my husband, the kindly and wise encouragement of two exceptional faculty mentors, the companionship of a group of “older” female students who shared much of what I felt, and the apparition of that “Goddess at the ER Door,” who evoked in me a determined reclaiming of compassion as a worthy vocation, I would likely not have found the will to endure.
And were it not for pediatrics, the one area in medicine to which I felt drawn. Pediatrics was one of the first medical disciplines to contemplate the fundamental “mind-body” connection. This was a field that had always grappled with the notions of “holistic” health and family centered care, because the interacting influences of nature and nurture on a child’s growth and development were too obvious to be ignored. Physical growth and strength, resistance to disease, acquisition of language, cognition, muscle skills, and social skills, were all greatly influenced by a child’s social and emotional environment, their family and community.
In children’s hospitals, “child life specialists” were beginning to engage children in art, music, play, and clowning, with a tacit acknowledgement that positive emotional experiences could enhance healing. Our hospital child life staff included a puppeteer, who also happened to work with Mr. Rogers of public television fame, and who happened to attend my Quaker meeting. I felt a tremendous gratitude for her gentle, affectionate presence on the pediatrics wards.
Most importantly, on the pediatric wards I found I could respond to my patients’ emotional needs and express more of my emotional self. If a child needed comfort, I could pick that child up, embracing my patient without meeting the disapproval of my work culture. In pediatrics, I caught a glimpse of what a more humane practice of medicine could look like, and I knew I had found the area of medicine I wanted to pursue.

In the intervening years, medical culture has come such a long way in recognizing emotional, mental, spiritual, and social contributions to health — to both the health of our patients as well as of that of ourselves, the providers. I now practice pediatrics, that discipline within medicine which had a head start in considering the whole patient, and I continue in my recovery of my whole self, slowly but steadily regaining my sense of myself as the whole provider.
I currently practice in Ethiopia. Here I am confronted with a different challenge to my capacity for compassion: the daily exposure to suffering that comes from extreme and disabling poverty. I look into the eyes of mothers who are unable to feed their children and see desperate hope that I will offer them some form of salvation. I feel the weight of their hope in me as a burden, knowing that what I can offer is small in the face of their need. The heaviness is lightened by many happy smiles of gratitude that do come my way, still it is depressing to be present to all the suffering. I do not want to close down, to not feel, but I often want to escape, to know the luxury of not seeing.
I see other brave clinicians, courageously putting in long hours over many years of charity care here and I marvel at them. None of this is easy for me, even after a year here. I have to work consciously at sustaining spiritual energy for compassion in this context. I meditate, I journal, I practice yoga, I garden, I play the piano. It helps greatly to have a cheerleader friend, Selamawit, the administrator of the clinic in the slum, who tells me everyday, “I appreciate you.” She keeps me going. It was with great interest that I listened to an interview with Roshi Joan Halifax. Krista Tippett posed to Joan the same question she has posed in several interviews:
“We are overwhelmed with a deluge of terrible news. The pictures are too present, too vivid, the news cycle too relentless. I see photos of children in faraway places that wreck me for a day. How do we be present to that and not be overwhelmed by it?”
This is my eternal question.
For me the images are not in photos, they are people in front of me daily, and they are, like Krista’s pictures, too vivid, too relentless. I face extreme want everywhere I go, walking on the streets of my neighborhood and driving in traffic. On my daily walk to and from the vegetable market I pass a corner where a mother and toddler, both dressed in dirty rags squat every morning to beg. The mother looks at me imploringly and prods the toddler to run up to me with his palm outstretched. I offer him a few strawberries or coins.
On my bicycle route to the orphanage where I make medical rounds once a week with the nurse, I pass a mound of trash piled four feet high on the side of road. A woman’s face stares straight out from about three feet up in the heap. She sits buried within her home, a mountain of trash, and observes the world passing by. A basket in front of the heap holds the few coins that passersby have tossed to her. I bike past the local Orthodox church and see groups of ragged children waiting for what handouts of bread that might come along with the alms offered to the regular church curb beggars.
In the van that I ride once a week to the U.S. Embassy clinic where I work, I look out the windows and see a beggar standing in the street at the window of the car ahead of the van. He is barefoot and his long bare skinny legs are thin poles, nothing more than skin and bone. His hair is matted with dirt and the ragged cotton gabi, a blanket which is thrown over his shoulders and trunk, made of white hand spun cotton, is so dirty that it is blackened. Under the gabi he wears nothing. He holds out his bony hand feebly. It shakes. Crowds of people stream along the sidewalk. No one takes notice of the starving beggar.

A young woman with a baby wrapped to her back winds her way between the bumpers toward the van. She reaches the van and steps up to the side window. The baby peers over her shoulder. There are flies crawling around the upper and lower lashes of his eyes. All the riders in the van stare straight ahead. She raps on the window but no one looks at her. Begging at car windows in the street is technically illegal in Ethiopia, so the employees of the U.S. Embassy have been instructed not to give to beggars when they are riding in embassy vehicles. She moves to the driver’s window, holds her palm out and then brings it to her mouth. The driver nods to her and mouths the words, Igzeeabirh yisitiling, may God give it to you for me, and she moves on.
On my drive to the clinic in the Kolfe slum where I see pediatric patients once a week, I pass a man in a wheelchair, his legs amputated above the knee. He is wheeling his way around the a traffic circle along with the cars. He keeps to the inner edge, squeezed between the inner lane of cars and the center cement guard rail and is facing my oncoming car so that the stubs of his legs, sticking out at the edge of the chair seat, appear head on like ragged circles under his torso. His arms are muscular, his jaw determined. Just beyond the circle I have to veer around what looks like a mound of old blankets along the edge of the center cement median. Bare feet stick out beyond the ragged blanket. The mound under the blanket with the feet sticking out has lain there for the past three days and has not moved.
I arrive at the clinic, and walk into the long open corridor where mothers and children wait to be seen, and all those eyes look up at me with my rolling suitcase full of medicines and supplemental foods. They smile and greet me welcomingly, their eyes full of hopeful supplication.
On a typical clinic day I will treat children with diarrhea and parasites, pneumonia, anemia, fungal and bacterial infections of the scalp and skin, and many who are undernourished, chronically stunted in height. Many of their mothers have no income or only the tiny income that comes from gathering firewood to sell.
My patients have included a three-year-old girl with protein malnutrition whose parents had been feeding her only potatoes and rice; several two-year-olds whose upper arm diameters were not much bigger than broom handles, still breastfeeding but not eating any supplemental foods. These children qualify for the Ethiopian government’s inpatient treatment for Severe Acute Malnutrition so we send them for admission.
Some children will be frightened and cranky but others are happy and playful, sensing no deprivation in their lives. The mothers are affectionate, kindly. There is much about their lives to cheer me, still it is the sadness in a mother’s eyes that will grab hold of me and haunt me.
Basic medications are very cheap here compared to in the U.S., but these parents cannot afford to buy them, so thanks to friends who contribute to a fund, I can supply them. We encourage mothers to start the babies on supplemental foods at six months (while continuing to breastfeed until two years). With the fund I am able to supply, for those who cannot afford to buy it, “Miten” a mix of 13 locally grown grains, pulses and seeds that has traditionally been used as a first complementary food.
Traditional Ethiopian crops make for a very nutritious diet. Lentils, chickpeas, teff, barley, flaxseed meal, safflower seeds, sesame seeds, carrots, cabbage, greens like collard greens all grow here. But most families living in the slum have no space to grow and cannot afford to buy these foods. They do not presently even have clean water to drink.
I found Roshi Joan’s terms in addressing Krista’s question so helpful. I see that I have experienced what she calls “empathic distress.” I have also experienced everything on her list of dysfunctional responses to empathic distress: the desire for flight, the avoidance, the moral outrage, the “vicarious trauma.”
I loved Joan’s metaphor for what it takes to survive a vocation for compassion when surrounded by suffering: buoyancy. “We need to stabilize ourselves in order to face the world with more buoyancy,” she said. Buoyancy is in fact what I need. The ability to rise up to the surface, to float, to bob there; not so much above it all, but still in it, just not drowned in it. Still able to see the sky, to breathe the air.
Hearing of her process for helping clinicians avoid dysfunctional responses to empathic distress has helped me to become more conscious of my own process, and I have incorporated some of her strategies: staying in touch with my body, “maintaining positive self regard.” I have come to see that when I am faced with a waiting room full of patients who themselves are likely hungry, it is really OK to break for a cup of tea and an oatmeal nut bar, if that is what I takes to keep me “buoyant.”

Like Joan, I have found silence to be medicine. I require a lot of silence to balance the chaos of that clinic in the slum. But the insight of the “truth of change, of impermanence” which, Joan told Krista, we come to understand when in a state of deep internal stillness, does not comfort me in this context. Joan said:
“The insight of impermanence liberates us from the futility of grief that disallows our own humanity to emerge.”
That sounds wonderful, but I wonder, would she say this if faced with a woman whose child is starving? The idea of impermanence of life does not matter in the life of a child. Now is what matters. There is such a thing as “too late,” in the life of a child. A child who is stunted by age two because of malnutrition, who is mentally dulled because of anemia, will suffer those effects for the rest of her life. Who cares about another life, a life after life, another reincarnation? The idea that we can experience liberation through understanding the impermanence of life sounds to me like one of those beautiful ideas that Jean Vanier might have been referring to when he said:
“As we share our lives with the powerless, we are obliged to leave behind our theories about the world, our dreams and our beautiful thoughts about God, to become grounded in a reality that can be quite harsh.”
Silence is medicine for me because it brings me the calm strength and focus that I need to face harsh realities. But it does not liberate me from experiencing grief over the harshness of those realities.
I also continue to contemplate Joan’s advice to “maintain distance between my self and my patient.” Everyone who offers helping advise to the helper professions speaks of the necessity of maintaining that distance. Of course there is an undeniable vast distance between my life and that of my patients here. I need no reminder to maintain physical boundaries. Like most privileged people I do so subconsciously, instinctively. I am ever faithful to my own precious privacy and health. But I do not wish to lose the ability to imagine life in my patients’ shoes, to feel what I would feel — if she were me — even though it is this empathic imagination that intensifies my pain.
I know that picking up a child, rocking her to comfort her crying, does as much if not more to alleviate my own discomfort as it does to address her suffering. But I also know that when Krista posed the question to Jean Vanier, “ How do we stand before pain?” he answered her that we do it bodily, in person, with someone in our own local world.
I realize I am comforting myself as well as these mothers and children when I give them the medicine or food they need. I could not bear to “care for” patients by writing a prescription that I knew would not be filled. I need to feel effective. I need gratification. I get it in seeing these children restored to health, beginning to grow again, and in their mothers’ pleasure at seeing them grow. I take great pleasure in seeing a child, who a month ago was sickly, irritable and underfed, now laughing and chasing me around the exam room.
Dr. Rachel Naomi Remen has said:
“To notice your joys instead of minimizing or discounting them is to become joyous. Notice joy, nourish joy, consciously take advantage of your opportunities to experience joy.”
This is the best advice I have found for surviving any work that places one in the midst of suffering. If there were not moments of joy I would be totally overwhelmed. I have to use my meditation time to dwell in that place where suffering has been relieved, and joy is on the faces of my patients. Joy is fuel for the journey.

This essay was originally submitted to the On Being blog in 2014. The author has since returned to the U.S. to practice medicine in North Carolina.

Share your reflection